Abstract
Introduction: Sepsis-associated disseminated intravascular coagulation (DIC) is a complex clinical syndrome with high mortality. The pathogenesis of DIC involves significant interactions between multiple pathophysiologic processes including coagulation, inflammation, infection response, platelets and endothelial dysfunction. The role of the endothelium in DIC is multifaceted and may contribute significantly to its severity and outcome. In sepsis, increased inflammation can lead to activation of the endothelium and the development of a procoagulant phenotype, characterized in part by elevated levels of cell surface tissue factor (TF). The endothelial response to inflammation is also characterized by the production of other factors that may be descriptive of the status of the endothelium, including endocan. The endothelium is also largely responsible for the production of endogenous anticoagulants, such as Tissue Factor Pathway Inhibitor (TFPI) and Protein C. The derangement of the endogenous anticoagulant system is critical to the pathogenesis of DIC and may also be reflective of the state of the endothelium. Investigation of factors that may prove damaging to the endothelium, including extracellular nuclear material such as nucleosomes and the protein High Mobility Group Box 1 (HMGB-1) may also provide insight into endothelial status and associated patient prognosis. The purpose of this study was to quantify measures of endothelial function, including markers of activation (TF and endocan), endogenous anticoagulants (TFPI and Protein C), and damage-associated factors (nucleosomes and HMGB-1) in the plasma of patients with sepsis and DIC and to determine the relationship of these factors with severity of illness and outcome.
Materials and Methods: Citrated plasma samples were prospectively collected from 103 patients with sepsis and suspected DIC at ICU admission (day 0) and again serially on ICU days 4 and 8 under an IRB approved protocol. DIC score was determined using the ISTH scoring algorithm (e.g. platelet count, PT/INR, fibrinogen, and D-Dimer). Plasma from healthy individuals was purchased from a commercial laboratory (George King Biomedical, Overland, KS). Plasma levels of endocan, TF, TFPI, nucleosomes, and HMGB-1 were evaluated using commercially available ELISA kits. Protein C levels were measured using a functional clot-based assay.
Results: In the DIC patients, endocan, TF, TFPI, nucleosomes, and HMGB-1 were significantly elevated compared to normal on ICU days 0, 4, and 8. Protein C was significantly reduced compared to normal at all time points.
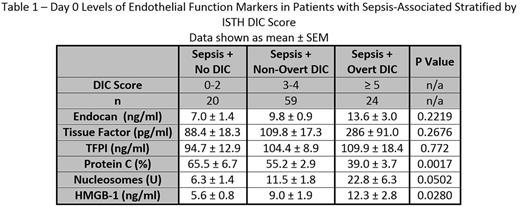
Patients were stratified into groups of sepsis and DIC based on the ISTH DIC score, and levels of markers were compared between groups. Markers reflective of overall endothelial activation (endocan and TF) showed no variation based on DIC score. Protein C showed significant variation based on DIC score, with a marked drop in Protein C levels with increasing severity of illness; however, TFPI showed no variation. Increasing levels of factors associated with endothelial damage (nucleosomes and HMGB-1) were observed with increasing severity of illness. Results are shown in Table 1.
Differences in biomarker levels between survivors and non-survivors were also evaluated. Endocan (p = 0.0252) and HMGB-1 (p = 0.0306) showed significant increases in non-survivors compared to survivors while Protein C showed a significant reduction (p = 0.0093) in non-survivors compared to survivors. TF, TFPI, and nucleosomes showed no variation based on survival.
Conclusion: Overall, levels of markers of endothelial activation, endogenous anticoagulants, and factors contributing to endothelial damage were elevated in the plasma of patients with sepsis-associated DIC compared to the healthy population. In particular, factors associated with endothelial damage, namely the toxic nuclear factors nucleosomes and HMGB-1, showed elevated levels with increasing severity of coagulopathy, suggesting that the endothelial damage caused by these factors may contribute to the development of coagulation dysfunction. Levels of endocan, Protein C, and HMGB-1 also showed significant association with mortality, underscoring the relevance of all aspects of endothelial physiology to patient outcome in DIC.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal